Understanding Tabernanthe Iboga and Its Origins
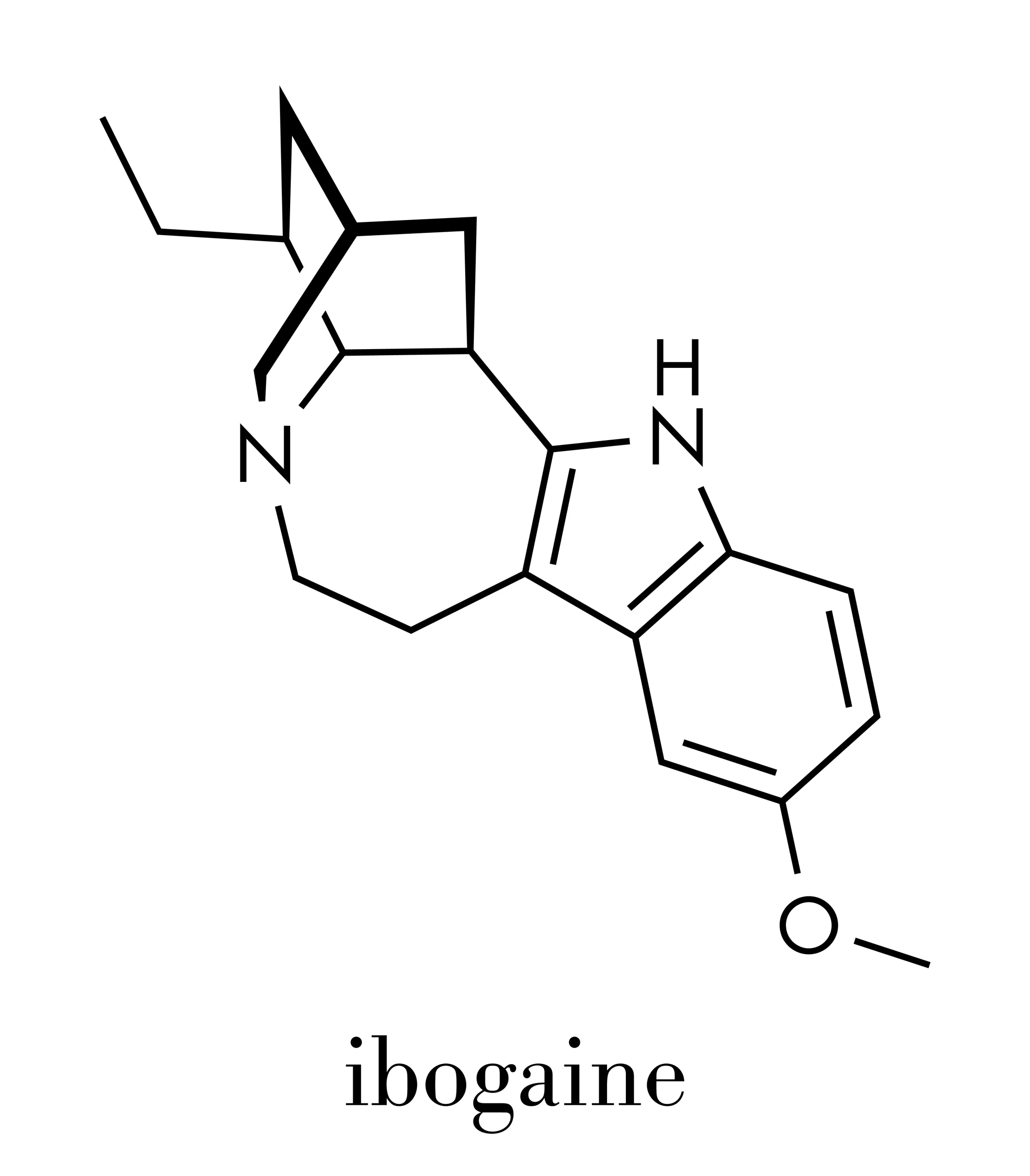
Ibogaine is a naturally occurring psychoactive compound extracted from the root bark of Tabernanthe iboga, a shrub native to Central and West Africa. For centuries, indigenous communities in Gabon and neighboring regions have used this plant in spiritual ceremonies and traditional healing practices. The Bwiti religion, in particular, considers iboga sacred, using it in initiation rituals and healing ceremonies.
The substance gained attention in the Western world during the 1960s when individuals experimenting with various substances noticed that ibogaine appeared to reduce withdrawal symptoms and cravings for opioids. This observation sparked decades of research into its potential applications for treating various forms of addiction, including alcoholism.
How Ibogaine Therapy Addresses Addiction
Ibogaine therapy works through multiple mechanisms that differentiate it from conventional addiction treatments. Unlike medications that require daily dosing, ibogaine is typically administered as a single treatment or a limited series of sessions. The compound interacts with numerous neurotransmitter systems in the brain, including serotonin, dopamine, and opioid receptors.
One of ibogaine’s most distinctive features is its ability to induce an intense introspective experience lasting several hours. During this period, patients often report revisiting traumatic memories, gaining insights into the psychological roots of their addiction, and experiencing a mental “reset” that reduces cravings. Physiologically, ibogaine appears to restore neurochemical balance disrupted by chronic alcohol use, potentially explaining the reduction in withdrawal symptoms many patients experience.
Research suggests that ibogaine may help interrupt the neural pathways associated with addictive behaviors, essentially giving the brain an opportunity to reorganize itself. This neuroplastic effect, combined with the psychological insights gained during the experience, may contribute to the treatment’s effectiveness.
Evidence for Ibogaine Treatment in Alcohol Use Disorder
The scientific evidence supporting ibogaine for alcohol use disorder is growing, but remains limited compared to established treatments. Several observational studies and case reports have documented promising outcomes.
- A 2017 study published in the American Journal of Drug and Alcohol Abuse followed individuals who received ibogaine treatment and found that participants reported significant reductions in alcohol consumption at follow-up periods ranging from one month to one year.
- Another study examining ibogaine’s effects on substance use disorders found that approximately 50-80% of participants reported reduced or eliminated alcohol consumption following treatment. These results are particularly noteworthy given that many participants had previously tried multiple conventional treatments without success.
However, it’s important to note that most existing research consists of small-scale studies, retrospective surveys, and anecdotal reports rather than large randomized controlled trials. The lack of rigorous clinical research stems partly from ibogaine’s legal status and the logistical challenges of conducting controlled studies with a Schedule I substance in countries like the United States.
The Addiction Treatment Process with Ibogaine
The addiction treatment process involving ibogaine differs significantly from traditional rehabilitation programs. Treatment typically takes place over several days and includes pre-treatment screening, the ibogaine session itself, and post-treatment integration support.
Before receiving ibogaine, patients undergo comprehensive medical and psychological evaluations. These assessments are crucial because certain pre-existing conditions can make ibogaine dangerous. Medical staff review cardiovascular health, liver and kidney function, and psychiatric history to identify any contraindications.
The actual ibogaine session usually lasts 24-36 hours, though the most intense effects occur during the first 8-12 hours. During this time, patients experience visual imagery, emotional processing, and physical sensations while remaining conscious. Medical staff monitor vital signs continuously throughout the experience.
Following the acute phase, patients typically remain at the treatment facility for several days of recovery and stabilization. Many programs also include counseling, integration therapy, and aftercare planning to help patients maintain their progress and address underlying psychological issues contributing to their alcohol use disorder.
The Critical Importance of Medical Supervision
Medical supervision during ibogaine treatment isn’t just recommended – it’s essential. Ibogaine can cause serious cardiac complications, including potentially fatal arrhythmias. The compound affects heart rhythm by prolonging the QT interval, which can lead to dangerous irregular heartbeats, particularly in individuals with pre-existing cardiac conditions or those taking certain medications.
Reputable treatment centers employ medical professionals who continuously monitor patients’ vital signs, including heart rate, blood pressure, and cardiac rhythm through EKG monitoring. They maintain emergency medical equipment and protocols to respond immediately to any complications. The presence of trained medical staff can mean the difference between a safe therapeutic experience and a medical emergency.
Unfortunately, not all facilities offering ibogaine treatment maintain adequate safety standards. Some clinics operate in countries with minimal regulatory oversight, and tragic fatalities have occurred when proper medical protocols weren’t followed. Anyone considering ibogaine treatment should thoroughly research facilities, verify their medical credentials, and ensure they have established safety protocols.
Understanding Potential Risks and Contraindications
The potential risks associated with ibogaine treatment extend beyond cardiac concerns. Individuals with certain medical or psychiatric conditions should avoid ibogaine entirely. These contraindications include heart disease, liver or kidney impairment, low blood pressure, seizure disorders, and certain psychiatric conditions such as schizophrenia or bipolar disorder.
Additional risks include nausea, vomiting, ataxia (loss of motor coordination), and temporary cognitive impairment during and after treatment. Some people experience prolonged psychological distress following ibogaine sessions, particularly if they aren’t adequately prepared for the intense introspective experience or lack proper integration support afterward.
Drug interactions pose another significant concern. Ibogaine can interact dangerously with many common medications, including antidepressants, antipsychotics, and cardiovascular drugs. Patients must fully disclose all medications and supplements they’re taking during pre-treatment screening.
The legal status of ibogaine also creates risks. In countries where it’s illegal or unregulated, patients have little recourse if they experience complications or substandard care. The lack of standardization means treatment quality varies dramatically between facilities.
Receive Evidence-Based Treatments for Alcohol Addiction Today!
Finding the right support can make all the difference. If you or someone you care about is struggling with alcohol addiction, our online directory connects you with trusted mental health providers who specialize in evidence-based treatment and compassionate care. Explore our directory today to compare providers, read profiles, and take the next step toward recovery with confidence.
Considering Ibogaine for Alcohol Abuse Treatment
For individuals struggling with alcohol abuse treatment who haven’t responded to conventional approaches, ibogaine represents a potential option worth investigating. However, it shouldn’t be viewed as a magic cure. Successful recovery from alcohol addiction typically requires ongoing support, lifestyle changes, and addressing underlying psychological issues.
Before pursuing ibogaine treatment, individuals should exhaust evidence-based approaches, including medically-supervised detoxification, behavioral therapies, mutual support groups, and FDA-approved medications like naltrexone, acamprosate, or disulfiram. These conventional treatments have established safety profiles and extensive research supporting their effectiveness.
If someone decides to explore ibogaine therapy after other treatments have failed, thorough research is paramount. This includes verifying the credentials and safety record of treatment facilities, understanding the full scope of risks, ensuring comprehensive medical screening will occur, and planning for aftercare and integration support.
Conclusion
Does ibogaine work for alcohol addiction? The evidence suggests it can be effective for reducing alcohol withdrawal symptoms, alcohol cravings, and alcohol dependence, though it’s not a guaranteed solution for everyone. This compound, called ibogaine, specifically ibogaine hydrochloride in its pharmaceutical form, works differently than a typical detox program by interacting with the brain’s neurotransmitters in unique ways. While Tabernanthe iboga acts as a mild stimulant in small doses, therapeutic ibogaine administration involves much larger amounts that produce profound psychological effects. Interestingly, ibogaine has shown promise not only for alcohol but also for drug dependence, drug use disorders, and opioid withdrawal, making it a subject of interest across multiple addiction fields.
However, one ibogaine treatment alone is rarely sufficient for long-term recovery from severe addiction. The treatment works best when combined with comprehensive aftercare, therapy, and lifestyle changes that address the root causes of substance use. Given the potential risks and the current limitations in research and regulation, ibogaine should be considered a last-resort option after conventional treatments have been exhausted, and only pursued at reputable facilities with proper medical oversight. As research continues and safety protocols improve, ibogaine may eventually become a more mainstream tool in addiction medicine. However, for now, it remains an experimental treatment that requires careful consideration and expert guidance.

About The Author
Dr. Sarah Johnson is a board-certified psychiatrist specializing in alcohol addiction and mental health care. She is dedicated to providing compassionate, evidence-based treatment that empowers patients to heal and build lasting resilience.
How to Find a Mental Health Provider That’s Right for You?
How to Know If You Need Therapy?
Psychiatrist vs Therapist: Which One Do You Need?
Teletherapy vs. In-Person Therapy: Which Is Better for You?
Does Insurance Cover Mental Health Treatment?
How Do I Know If I Need Therapy?